Comprehensive Layout for Exploration Analysis & Research [CLEAR] Claims
Built on the foundation of one of the most comprehensive claims data sets in the nation, PurpleLab® Comprehensive Layout for Exploration Analysis & Research (CLEAR Claims) makes market and clinical utilization research easy by combining our data & methodologies into easy-to-use, in-platform solutions. CLEAR claims facilitates faster analysis and reduces the amount of data engineering needed to use claims data.
Expect more than vended claims. PurpleLab adds value to all the data we aggregate, populating it into use-case driven toolsets and making access to the data easy.
About PurpleLab® CLEAR Claims
CLEAR Claims is designed for users that need access to comprehensive patient claims data at a detailed level and simplifies querying. Through clinically approved and operationally relevant methodologies, we identify the underlying reason for a visit or admission with payer and provider attribution. Users access enhanced claims data with final claims in consolidated table structures for quicker analysis.
We've done the work to make the data usable within minutes. Let us help you unlock the full potential of your patient claims data. Get in touch with us today and discover how CLEAR Claims enhances RWD capabilities and can optimize the way you analyze and interpret your healthcare data. Additional information is available on our resources page.
Looking to get a an idea of what CLEAR Claims looks like?
View this short video to learn even more about CLEAR Claims capabilities.
Here’s all the good stuff

Methodologies
Give you the flexibility to decide which insights you need from the data.

Speed & Delivery
Your data will be ready for use in minutes, available through your preferred delivery method. See what you need in one place.

Linkage
We can link datasets and have relationships to help you with expert determination.

Usability
PurpleLab provides data in an easy-to-use, common data model that reduces the required data engineering.
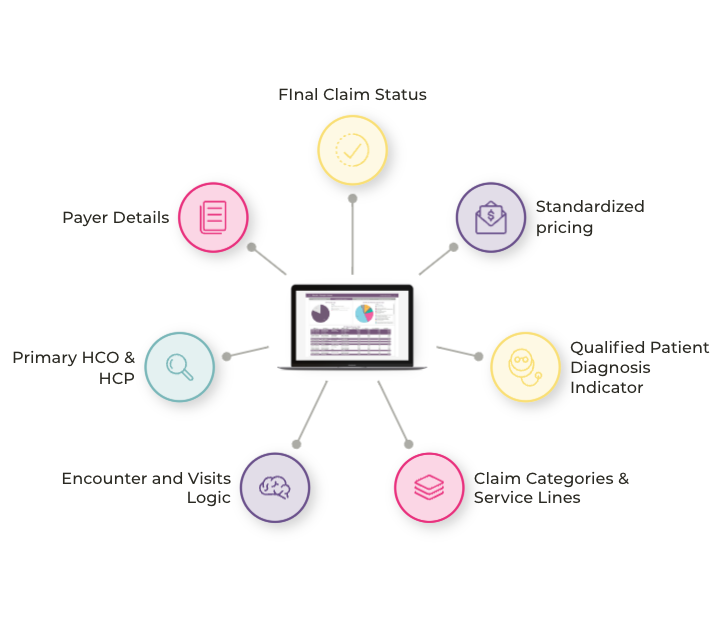
Payer & Provider Core Methodologies
Encounter Logic
Establish operational counting stats by linking related claims into admissions for inpatients and splitting bundled claims into visits for other contexts.
Standardized Pricing
Access pricing for services provided on the claim based on enhanced CMS fee schedules and payer-type mark-ups for medical claims.
Primary HCP/HCO Identification
Understand the most relevant doctor or facility associated with a claim based on a hierarchy of provider roles.
Additional Methodologies
Utilize claim level classifications based on a hierarchy of underlying services or service locations.
Identify resubmissions of the same service for a patient to eliminate duplicate or restated claims.
Access primary and secondary payer information, including payer name and channel/sub channel for Mx and MCO issuer for Rx.
Identify claims where the diagnosis code supports the identification of a patient's condition.